For generations, the world of healthcare has been a landscape of profound paradoxes. It is an industry of breathtaking scientific innovation, capable of transplanting organs and editing the very code of life. Yet, it has remained, in many ways, a cottage industry of fragmented, paper-based, and stubbornly analog workflows. It is a world of deep, human-centric care, yet also one of immense administrative friction, of data trapped in siloed systems, and of a patient experience that is often frustratingly disconnected. This long era of digital lag is now giving way to one of the most significant and consequential transformations in modern history.
We are in the midst of a monumental and accelerating expansion of the healthcare software ecosystem. This is not just a story about hospitals finally adopting electronic health records; it is a story of a complete and holistic “digitalization” of the entire healthcare value chain. A new and powerful ecosystem of interconnected software, data, and devices is emerging, a “connected pulse” that is breaking down the old silos, empowering both patients and providers with unprecedented access to information, and paving the way for a new era of medicine that is more personalized, more proactive, and more participatory than ever before. From the foundational EHR platforms in the hospital to the AI-powered diagnostic tools in the cloud, and the consumer-facing wellness apps on our smartphones, this expanding software ecosystem is not just an adjunct to healthcare; it is becoming the very nervous system of healthcare itself.
The Burning Platform: The Powerful Forces Driving the Digital Transformation of Healthcare
The rapid and system-wide expansion of the healthcare software ecosystem is not a technology-led phenomenon. It is a necessary and urgent response to a “perfect storm” of powerful economic, demographic, and societal pressures that have made the old, analog healthcare model unsustainable.
Understanding these foundational drivers is key to understanding the “why” behind this massive and irreversible digital shift.
The Unsustainable Cost Crisis
In nearly every developed country, healthcare spending is growing at a rate far outpacing economic growth, consuming an ever-larger share of national GDP.
- The Inefficiency of Manual Processes: A large portion of this cost is driven by the immense administrative inefficiency of a system that is still heavily reliant on manual, paper-based workflows, from patient scheduling and billing to the endless duplication of tests and forms resulting from a lack of data sharing.
- The Shift to Value-Based Care: The traditional “fee-for-service” model, in which providers are paid for the volume of services they deliver, is slowly giving way to a “value-based care” model, in which providers are compensated based on their patients’ health outcomes. This creates a powerful financial incentive to invest in the software and data analytics needed to manage patient health and prevent costly hospitalizations proactively.
The Demographic and Epidemiological Shifts
The world is getting older, and the burden of chronic disease is growing.
- The “Silver Tsunami”: The aging of the global population is leading to a massive increase in the prevalence of chronic diseases like diabetes, heart disease, and cancer. These are conditions that require continuous, long-term management, not just episodic, acute care.
- The Need for Continuous and Remote Care: The management of these chronic conditions is a perfect fit for the new, digitally enabled models of care, such as remote patient monitoring (RPM), which allow a patient’s vital signs to be tracked from home using connected devices.
The Revolution in Customer (Patient) Expectations
The modern patient is also a modern consumer. They are conditioned by the seamless, on-demand, and personalized experiences they get from every other industry, and they are now bringing those same expectations to their healthcare.
- The Demand for Convenience and Access: Patients are no longer willing to tolerate long wait times, inconvenient appointment scheduling, and endless paperwork. They want the same kind of “on-demand” convenience from their healthcare that they get from Amazon or Uber.
- The Rise of the Empowered “e-Patient”: The internet has created a new generation of informed and empowered “e-patients” who actively research their conditions and want to be engaged partners in their own healthcare journey. They are demanding access to their own health data and the digital tools to help them manage it.
The Explosion of Health Data
We are in the midst of a “big bang” of health data generation.
- The “Digitization” of the Clinical Record: The widespread adoption of Electronic Health Records (EHRs) has transformed the patient’s clinical history from an illegible paper chart into a massive, mineable digital dataset.
- The Genomic Revolution: The cost of sequencing a human genome has plummeted, creating a new and incredibly rich layer of personal health data.
- The “Quantified Self” and Wearable Data: A huge and growing stream of real-world health and wellness data is now being generated outside of the clinic, from the heart rate sensors on our smartwatches, the sleep trackers on our rings, and the data from our connected glucometers and blood pressure cuffs.
This “data tsunami” is both a massive challenge and a massive opportunity. The healthcare software ecosystem is the essential infrastructure needed to collect, integrate, and, most importantly, make sense of the vast and diverse new world of health information.
The Catalyst of the COVID-19 Pandemic
The COVID-19 pandemic was a massive, unprecedented catalyst that served as a “time machine” for the adoption of digital health, compressing a decade’s worth of change into months.
- The Telehealth Explosion: With in-person visits shut down, the healthcare system was forced to adopt telehealth and virtual care models almost overnight. This proved to both patients and providers that high-quality care could be delivered remotely, and it broke down many of the longstanding regulatory and reimbursement barriers that had held telehealth back.
- The Acceleration of Remote Patient Monitoring: The need to monitor COVID-19 patients at home led to a massive acceleration in the adoption of RPM technologies.
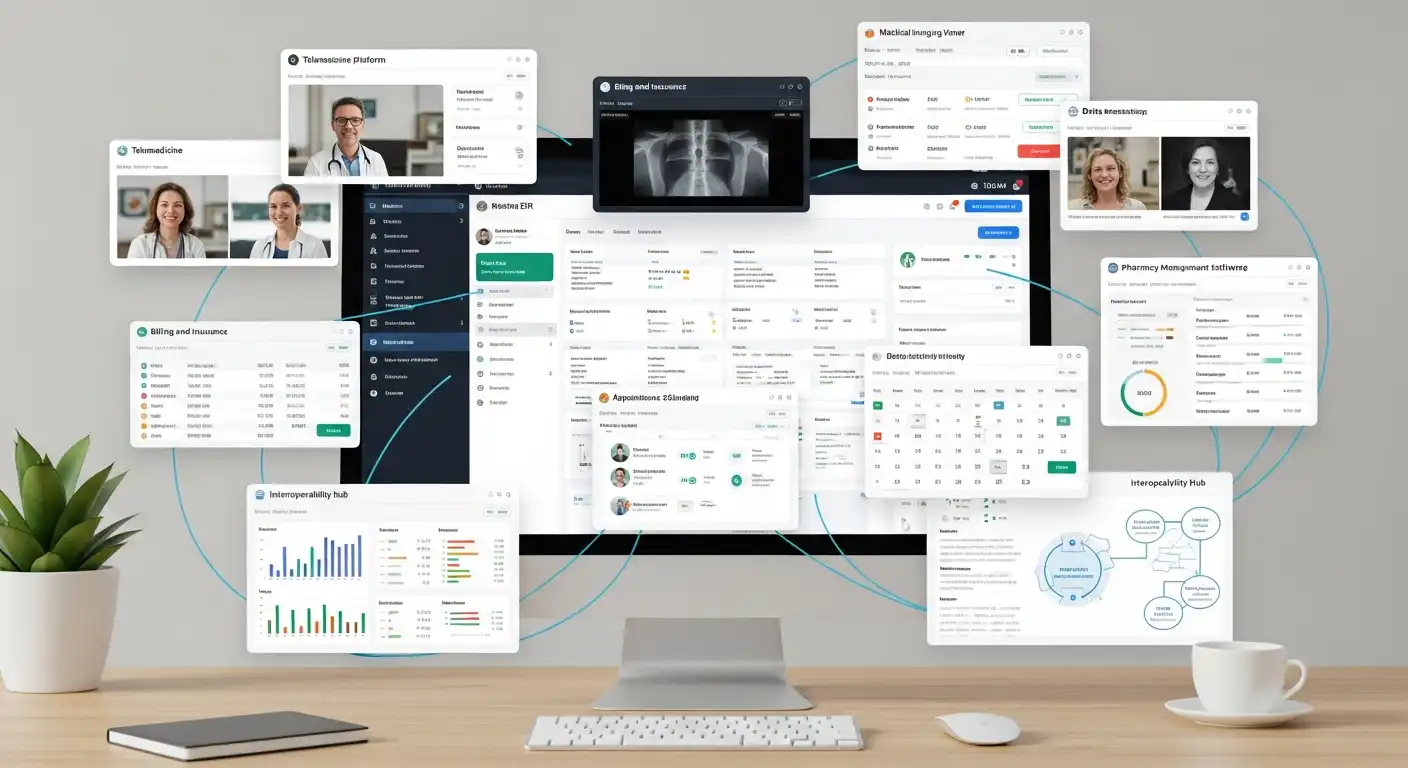
The Anatomy of the Modern Healthcare Software Ecosystem: A Multi-Layered Landscape
The modern healthcare software ecosystem is not a single, monolithic entity. It is a complex, multi-layered, and increasingly interconnected landscape of different software categories, each serving a specific role in the patient’s and the provider’s journey.
Let’s explore the key “layers” of this new, connected architecture, from the foundational systems in the hospital to the new, patient-facing applications on our phones.
The Foundational “Systems of Record” – The Clinical and Administrative Core
This is the traditional heartland of healthcare IT, the mission-critical, enterprise-grade systems that run the core clinical and administrative operations of the hospital and the large health system.
These are the “heavyweight” platforms that serve as the ultimate “source of truth” for the patient’s official medical and financial records.
- The Electronic Health Record (EHR) / Electronic Medical Record (EMR):
- The Core Function: The EHR is the digital version of the patient’s paper chart. It is the central legal record of a patient’s clinical history, diagnoses, medications, lab results, and treatment plans. It is the primary software that doctors and nurses use in their daily workflow.
- The Landscape: The EHR market is massive, but it is dominated by a handful of large, incumbent vendors, particularly Epic Systems and Cerner (now part of Oracle), which together control a large share of the U.S. hospital market. Other major players include MEDITECH and Allscripts.
- The Challenge and the Evolution: While the adoption of EHRs has been a critical step in digitizing healthcare, these first-generation systems are often criticized for their clunky user interfaces, poor interoperability, and their contribution to physician burnout. The new frontier for EHRs is making them more open, intelligent, and user-friendly.
- The Practice Management (PM) System: The PM system is the administrative and financial counterpart to the EHR. It manages the “business” of the medical practice, including patient scheduling, registration, and, most importantly, the complex process of medical billing and claims processing.
- The Radiology Information System (RIS) and Picture Archiving and Communication System (PACS): These specialized systems manage the workflow and images for the radiology department, from scheduling an MRI to storing and viewing digital images.
The “Systems of Engagement” – The New Digital Front Door
This layer of the ecosystem is focused on the direct interaction between the patient and the healthcare system. This is the new “digital front door” of healthcare.
This is a hotbed of innovation, with a new generation of software that is creating a more convenient, accessible, and consumer-centric healthcare experience.
- The Telehealth and Virtual Care Platforms:
- The Core Function: These platforms provide the software and the infrastructure for conducting secure, HIPAA-compliant video consultations between patients and providers.
- The Landscape: The telehealth market exploded during the pandemic, with standalone players like Teladoc and Amwell seeing massive growth. We are also seeing this functionality being deeply integrated into the core EHR platforms and the patient portals.
- The Patient Portal and the Digital Front Door Platform:
- The Core Function: The patient portal is the secure website or mobile app that gives a patient access to their own health information (from the EHR), the ability to communicate securely with their doctor, to schedule appointments, and to pay their bills.
- The Evolution: The simple patient portal is evolving into a more comprehensive “digital front door” platform that aims to be the single, integrated entry point for all of a patient’s digital interactions with a health system.
- Remote Patient Monitoring (RPM) Platforms:
- The Core Function: These platforms are the software that connects to a patient’s in-home medical devices (like a connected blood pressure cuff, a glucometer, or a smart scale). The platform collects data from these devices, sets alert thresholds, and provides a dashboard for a clinical team to monitor the health of a large patient population remotely.
The “Systems of Intelligence” – The AI and Analytics Layer
This is the most exciting and fastest-evolving layer of the ecosystem. This is the “brain” that uses the vast amounts of data generated by the other systems to create a new, more intelligent, and more predictive form of medicine.
- Clinical Decision Support (CDS):
- The Core Function: CDS tools are integrated directly into the clinician’s workflow (often within the EHR) to provide real-time, evidence-based guidance at the point of care. This could be an alert about a potential drug interaction or a recommendation for a specific diagnostic test based on the patient’s symptoms and history.
- The AI-Powered Evolution: The next generation of CDS is being powered by AI. An AI-powered CDS could analyze a patient’s entire medical history and the latest clinical research to provide a much more sophisticated and personalized set of recommendations.
- AI in Medical Imaging:
- The Core Function: This is one of the most mature and impactful applications of AI in healthcare. AI-powered computer vision algorithms are used to analyze medical images (such as X-rays, CT scans, and MRIs) to assist radiologists in detecting diseases like cancer, stroke, and lung disease.
- The Impact: These AI tools can often detect subtle patterns invisible to the human eye and serve as a powerful “second opinion,” improving the accuracy and speed of the diagnostic process.
- Population Health Management (PHM) and Predictive Analytics:
- The Core Function: PHM platforms are used by healthcare organizations (particularly those in value-based care contracts) to manage the health of entire patient populations.
- The Role of AI: These platforms use AI and machine learning to analyze large datasets of patient information to identify high-risk individuals most likely to experience a costly medical event in the future (e.g., a patient at high risk of a hospital readmission). This allows the health system to proactively intervene with these high-risk patients, providing the care and support they need to stay healthy and out of the hospital.
The Consumer-Facing Health and Wellness Ecosystem
This is the massive and rapidly growing ecosystem of direct-to-consumer digital health apps and wearable devices. While this layer often exists outside of the traditional healthcare system, the lines are beginning to blur.
- The Wearable and “Quantified Self” Revolution: The proliferation of consumer wearable devices from companies like Apple, Google (Fitbit), and Oura is creating a massive new stream of real-world, longitudinal health data.
- The Digital Therapeutics (DTx) Market: A new, FDA-regulated category of software is emerging. A DTx is a software-based intervention that is designed to treat or manage a medical condition. For example, there are now FDA-cleared DTx apps that can deliver cognitive behavioral therapy (CBT) for depression or help a patient manage their diabetes.
- The Bridge to the Clinical World: The biggest challenge and opportunity in this space is integrating consumer-generated health data with clinical data in the EHR. When a doctor can see not just the patient’s blood pressure reading from their annual physical but also their continuous blood pressure trend over the past six months from their wearable device, it opens up a whole new world of proactive, personalized care.
The Interoperability Imperative: The Quest for a Truly Connected Ecosystem
The single greatest challenge, and the most important trend, in the entire healthcare software landscape is the quest for interoperability.
Interoperability is the ability of different information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated manner. It is the holy grail needed to break down data silos and create a truly seamless, connected healthcare ecosystem.
The Decades-Long Struggle for a Common Language
For decades, the healthcare industry has been a “digital Tower of Babel.” Every EHR vendor, every medical device, and every lab system spoke its own proprietary language and used its own proprietary data formats. This lack of a common language has been the primary barrier to data sharing.
The Rise of FHIR: A Modern, API-First Standard for Healthcare Data
A major and revolutionary breakthrough in this struggle has been the development and the widespread adoption of a new data standard called FHIR (Fast Healthcare Interoperability Resources), pronounced “fire.”
FHIR is a modern, web-based standard for exchanging healthcare information electronically.
- The FHIR Philosophy: FHIR was developed by the standards organization HL7 International, and it is built on the same modern, API-first principles that power the rest of the consumer internet. It uses common web standards, such as RESTful APIs, and represents data in a simple, easy-to-use JSON format.
- The Impact of FHIR: FHIR is a game-changer. It makes it dramatically easier for developers to build applications that can securely access and exchange data with EHRs and other clinical systems. It is the “API for healthcare” that the industry has been waiting for.
- The Regulatory Push: The adoption of FHIR has been massively accelerated by government regulation. In the U.S., the 21st Century Cures Act is a landmark piece of legislation that mandates that EHR vendors provide a standardized, FHIR-based API that allows patients to access their health data through the third-party app of their choice. This is the rule that has enabled a new ecosystem of consumer-facing health apps that can plug directly into patients’ official medical records.
The “App Store” for Healthcare: The New Platform Ecosystems
The rise of FHIR and new regulatory mandates for open APIs are enabling the creation of a more open, innovative platform ecosystem for healthcare, analogous to the app stores of the mobile world.
- The EHR as a Platform: Major EHR vendors, such as Epic and Cerner, are now rebranding themselves as open platforms. They have launched their own “app stores” (the Epic App Orchard and the Cerner CODE Program) where third-party developers can build. Market applications that are pre-integrated with the EHR and that can be “plugged in” by a hospital to add a new capability, such as a specialized clinical workflow tool or a new telehealth service.
The Future of the Healthcare Software Ecosystem: The Path to an Intelligent, Ambient, and Personalized Future
The expansion and the evolution of the healthcare software ecosystem are not slowing down; they are accelerating. The trends of today are all pointing towards a future of healthcare that is more intelligent, more automated, more seamlessly integrated into our lives, and more deeply personalized to the individual.
The Rise of the “Ambient Clinical Intelligence”
One of the biggest sources of physician burnout is the immense administrative burden of the EHR, the need to spend hours clicking boxes and typing notes. The next frontier is “ambient clinical intelligence.”
- The Vision: An exam room where an AI-powered, ambient-listening device can securely and unobtrusively listen to the natural conversation between a doctor and a patient. The AI would then automatically and intelligently transcribe the conversation and populate the relevant fields of the EHR in real time.
- The Impact: This would be a revolutionary leap in usability. It would free the doctor from the tyranny of the keyboard, allowing them to focus their full attention on the human connection with the patient. Companies like Nuance (owned by Microsoft) and Suki are the leaders in this space.
The “Digital Twin” of the Patient
As we have seen, the ultimate vision for personalized and predictive medicine is the creation of a “digital twin” for each patient.
This living, breathing virtual model of a person’s health would be continuously updated with their clinical and genomic data, as well as real-time data from their wearable devices. This would be the ultimate platform for simulating the effects of different treatments and for providing a new level of proactive, predictive healthcare.
The Decentralization of Care and the “Hospital at Home”
The healthcare software ecosystem will be the key enabler of a massive shift in the “site of care,” moving a significant amount of care from the expensive, centralized hospital to the comfort and convenience of the patient’s home.
The “hospital at home” model, combining telehealth, remote patient monitoring, and in-home services, will be orchestrated by a sophisticated, cloud-based software platform.
The Challenges on the Road to a Fully Connected Future
For all its immense promise, the path to a fully realized, intelligent, and interconnected healthcare software ecosystem is not without significant and formidable challenges.
The Cybersecurity and Privacy Imperative
Healthcare data is among the most sensitive and personal data, and healthcare organizations are prime targets for cybercriminals. Securing this sprawling, interconnected ecosystem is a massive, non-negotiable challenge. The privacy and security of patient data must be the absolute, foundational priority of any new technology introduced.
The Challenge of Physician Burnout and Workflow Integration
A new piece of software, no matter how powerful, is a failure if it adds to the already crushing workload of a doctor or a nurse. The biggest lesson from the first generation of EHRs is that technology must be designed to fit seamlessly into the clinical workflow, not the other way around. The user experience and the “clinician experience” must be a top-level design priority.
The Data and AI Governance Gauntlet
As AI becomes more deeply embedded in clinical decision-making, it brings a host of new and complex challenges in governance, ethics, and accountability. How do we ensure that the AI models are not biased? How do we validate their safety and efficacy? Who is liable when an AI-powered system makes a mistake? These are the profound questions that regulators, health systems, and technology companies are now grappling with.
The Need for New Skills and a Digital-Ready Workforce
The healthcare workforce of today was not, for the most part, trained for this new, digital-first world. There is a massive and urgent need to reskill and upskill the entire clinical workforce, from doctors and nurses to medical assistants, to be comfortable, confident, and competent in using these new digital tools.
Conclusion
The global healthcare industry is in the early stages of a once-in-a-century transformation, a profound shift from an analog, fragmented, and reactive system to a digital, connected, and proactive one. The expanding healthcare software ecosystem is the essential, indispensable “operating system” for this new era. It is the connective tissue that is breaking down old silos, the intelligent engine that is turning a flood of data into life-saving insights, and the new digital front door that is creating a more empowered, consumer-centric relationship between the patient and their health.
The journey ahead is long and complex, filled with immense technical, regulatory, and cultural challenges. But the destination is a future of healthcare that is more personalized, more predictive, more equitable, and more deeply human. The companies and the health systems that are building and embracing this new, connected pulse are not just creating better software; they are building a healthier future for all of us.